Prioritising osteoarthritis
Osteoarthritis is common and particularly so in people aged 45 years and older. It causes joint pain and stiffness and, consequently, problems with mobility and function. These symptoms, which occur most frequently in knees, hips, hands/wrists and feet/ankles, can result in negative outcomes such as lost days from work, inability to undertake caring duties, poor sleep and reduced quality of life. Traditionally, osteoarthritis has been poorly prioritised by healthcare professionals and patients, driven, in part, by the misunderstanding that there is little that can be done for the condition. We now know that inevitable decline is not to be expected, that osteoarthritis is linked with worse health outcomes (including cardiovascular disease and death), that there are effective core treatments (exercise and weight control) that can improve pain and function yet healthcare professionals and patients under-use these core treatments and continue to over-rely on drug-based treatment which carry greater risks without associated enhanced benefits. Finally, we know that x-rays and joint replacements are over-used in the diagnosis and management of osteoarthritis, internationally. Prioritisation of high-quality, evidence-based management of osteoarthritis therefore has potential to improve patient outcomes, quality of life, societal burdens and reduce imaging and surgical resources.
The global burden of osteoarthritis
Globally, osteoarthritis has been rising as one of the leading causes of years lived with disability both due to its functional effects and high world-wide prevalence. In the UK alone, 8.75 million people have sought treatment for osteoarthritis and frequent consultation rates for osteoarthritis are consistent internationally. Given this high global burden, even small improvements at an individual level in primary care have potential for significant population-level benefits.
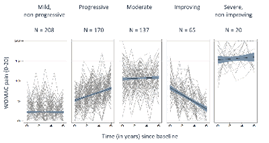
It is a myth that osteoarthritis inevitably gets worse. We now know that various patterns for patient symptoms exist, including a group who has mild, non-progressive symptoms. Flares, which are often characterised to patients as a worsening of their symptoms (such as pain), are common and can last for a variable length of time. Although pain and disability can be, or become, significant for some patients, joint replacement is not the eventual outcome for most patients. However, if joint replacement is needed, it has good outcomes for most patients.
Osteoarthritis commonly occurs alongside conditions such as cardiovascular disease, diabetes, obesity and depression. Further, among all patients with two or more long-term conditions, osteoarthritis is commonly one of these. This is problematic for a number of reasons, firstly, pain and mobility problems can present barriers to patients engaging completely with self-management for commonly co-existing problems, such as high blood pressure, heart disease, obesity, diabetes or respiratory problems (e.g. asthma or chronic obstructive pulmonary disease). Thus, there is potential for the patient to enter into a vicious cycle of worsening symptoms and even less chance of engaging in self-management which will have a negative impact on both their osteoarthritis and these other conditions. Secondly, pain and loss of function resulting from osteoarthritis, this can affect both mood and sleep, potentially worsening outcomes of commonly co-existing mental health problems. Again a vicious cycle ensues as symptoms can amplify among those with low mood and anxiety. Finally, the current over-reliance on drug treatments can negatively impact other conditions, for example, anti-inflammatories can worsen blood pressure control and can have negative effects on kidney function and opioids have been linked to increased risk of cardiovascular disease.

Osteoarthritis is associated with many negative consequences for patients, the population and society. Not least, osteoarthritis is consistently found to have a negative impact on patients’ quality of life. There are multiple contributors to this, including pain, reduced ability to function, low mood and fatigue. Further, misconceptions about osteoarthritis exist, for example that pain is an indicator of damage being caused, can create anxiety among patients when they try and self-manage the condition as exercise-related pain is common. Another myth is that some patients believe that osteoarthritis will inevitably worsen, our evidence suggests this is inaccurate, however, it can undermine efforts to support self-management of the condition.
Recommended care and NICE guidance
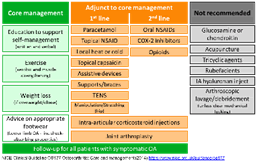
The National Institute for Health and Care Excellence (NICE) has recommended core, evidence-based management approaches that should be undertaken for everyone with osteoarthritis and a suite of approaches that can be used to support patients to undertake core treatment and manage their symptoms.
Core treatment for osteoarthritis includes supported self-management:
- Access to appropriate information e.g. the Keele University Osteoarthritis Guidebook and Versus Arthritis patient information leaflets
- Advice to exercise – both general aerobic fitness and local muscle strengthening exercises (for examples, those outlined by Versus Arthritis)
- Weight loss (if overweight or obese, that is, the patient has a Body Mass Index (BMI) of ≥25)
- Advice on appropriate footwear in the presence of lower limb osteoarthritis
First line adjuncts to core treatment approaches include:
- Drug-based approaches: paracetamol, topical non-steroid anti-inflammatories (NSAIDs), topical capsaicin
- Non-drug-based approaches: local heat or cold, assistive devices, supports/braces, transcutaneous electrical nerve stimulation, manipulation/stretching (for hip osteoarthritis)
Second line adjuncts to core treatment approaches include:
- Oral non-steroidal anti-inflammatories (NSAIDs), cyclo-oxygenase-2 (COX-2) inhibitors, opioids
In addition to these recommendations, intra-articular corticosteroid injections can be considered to support use of core treatments and joint arthroplasty can be considered if core management has been offered without adequate benefit.
Review and follow-up of all patients with symptoms of osteoarthritis is recommended, timed according to the needs of the individual patient.